Churches. Hair salons. Restaurants. Malls. What do they all have in common?
They’ve all been cleared to reopen in San Diego County amid the ongoing coronavirus pandemic — and by and large, they all require people to congregate inside, potentially with strangers.
This comes as an increasingly vocal group of scientists has sounded the alarm about the danger of indoor gatherings due to the potential for airborne transmission of the disease by “super-spreaders.”
This week Kimberly Prather of UC San Diego’s Scripps Institution of Oceanography penned an urgently worded perspective paper in the journal Science saying as much. She asserted, as an atmospheric chemist, that a thorough review of the existing literature provides strong evidence that the new coronavirus can linger in the air, perhaps for hours, before slipping deep into a person’s lungs.
Local and state health officials have put in place strict guidelines for businesses and churches that want to reopen in San Diego. Social distancing is required, which will limit the number of patrons that can pack into any particular venue. And while barbershops and salons were allowed to open, procedures that require workers to touch a client’s face — such as eyelash services, eyebrow waxing and facials — as well as nail salons remain prohibited.
Several San Diego area tribal casinos also have opened, despite opposition by Gov. Gavin Newsom.
Temperature checks and routine health screenings of workers are mandatory under the guidelines. Restaurants are encouraged to provide outdoor seating whenever possible, but it’s not a requirement. It’s also not required that restaurant goers wear masks while seated.



Friends begin with a toast before dinner underneath a cabana at One Door North restaurant in North Park on Friday. This was their groups first dinner outing together since the coronavirus pandemic.
(Nelvin C. Cepeda / The San Diego Union-Tribune)
The report by Prather and other researchers was largely a plea for people to use face masks. But the larger message was, think twice before you hang out in public too long, especially in enclosed spaces.
Prather specifically highlighted recent research that has suggested many coronavirus infections can be traced back to a small number of people. These super-spreaders, for whatever reason, appear to be able to walk into a bar, restaurant or church, and simply by chatting or singing infect many people around them.
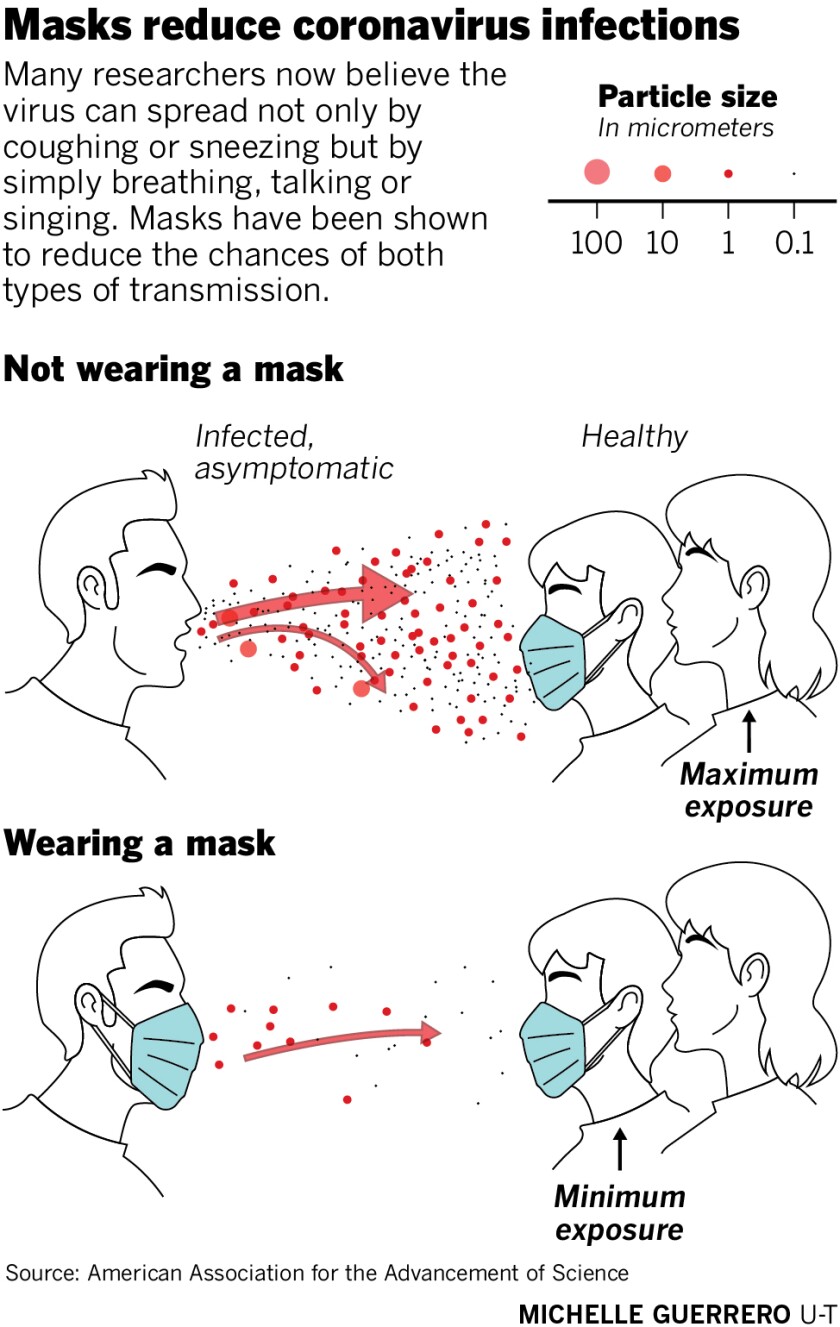
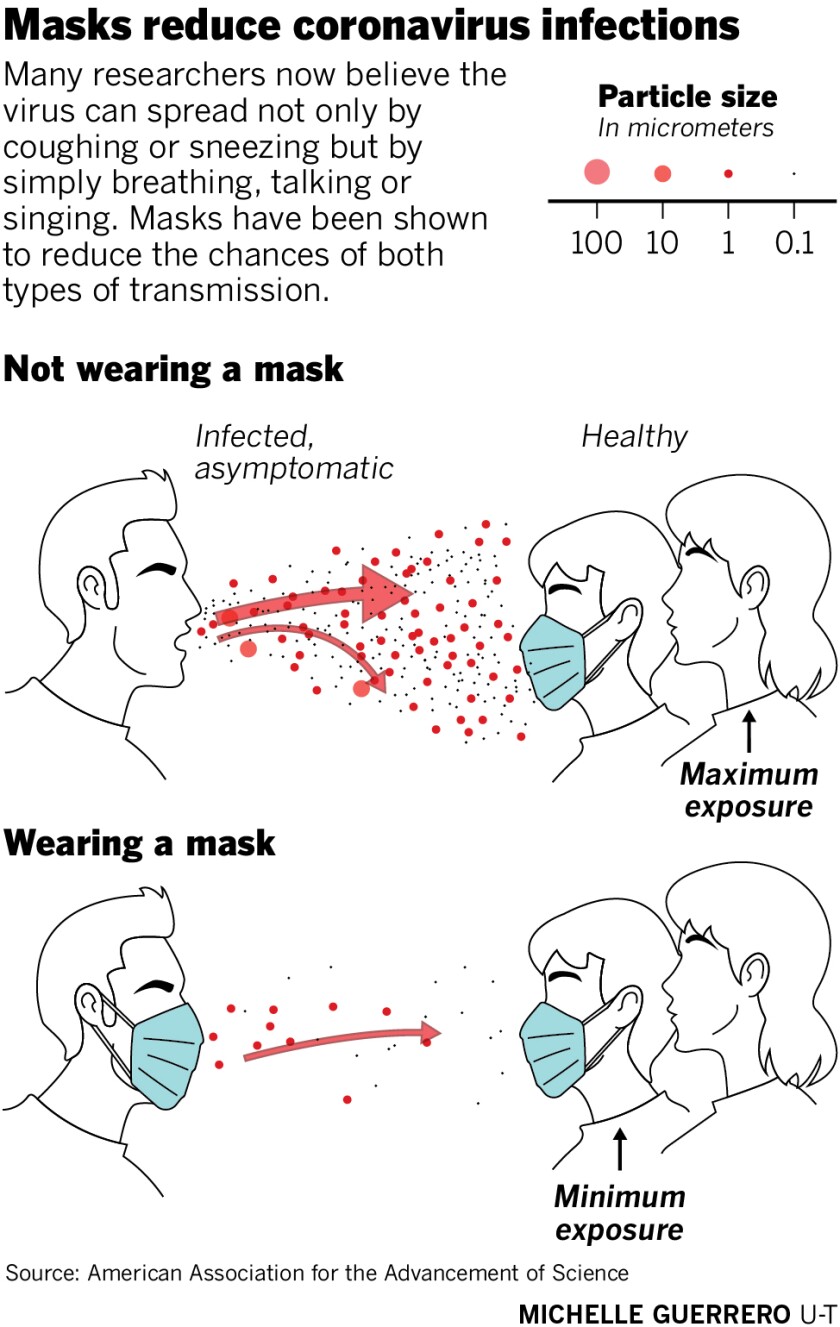
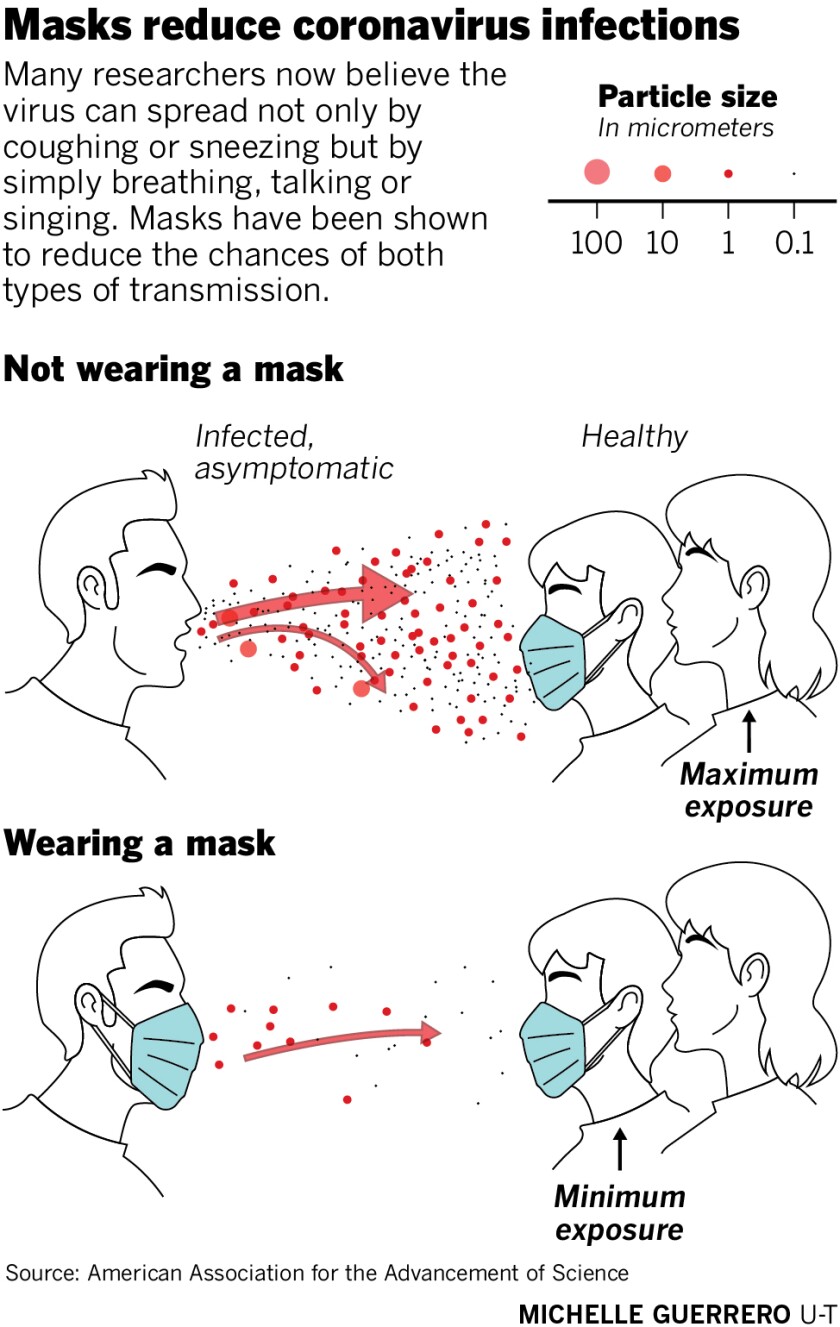
“Evidence suggests that SARS-CoV-2 is silently spreading in aerosols exhaled by highly contagious infected individuals with no symptoms,” the paper concluded. “Owing to their smaller size, aerosols may lead to higher severity of COVID-19 because virus-containing aerosols penetrate more deeply into the lungs.”
The science isn’t settled on super-spreaders or whether aerosols can pack a viral punch strong enough to infect and kill people. While some researchers have argued that there’s enough evidence to warrant immediate action, others have said there’s a lack of definitive studies.
Still, the emerging science was enough to get the attention of Dr. Robert Schooley, an infectious disease expert at the UCSD School of Medicine. He coauthored the paper with Prather and is genuinely concerned about the airborne spread of the virus and disregard for face coverings.
“If you want to be successful in going back to work and going back to school, wearing a mask is the best way to ensure that experiment is successful,” he said. “If you want to have it fail, go to restaurants and don’t wear masks and yell at each other across the table.”
Prather was caught up in a controversy just last month after she warned people publicly about the dangers of congregating at the beach. She had to clarify that her theory that the coronavirus could spread through ocean water polluted with sewage, something of which San Diego has no shortage, was still just a hypothesis and not settled science.
San Diego County Public Health Officials declined to comment on the potential for airborne transmission, other than to repeatedly cite its absence in federal guidance. The Centers for Disease Control and Prevention doesn’t officially recognize airborne transmission of the virus as a significant threat; nor does the World Health Organization.
“We are going with the current evidence,” said Dr. Wilma Wooten, county public health officer, during a press briefing on Thursday. “As new evidence comes available, we will take the necessary actions, but right now we’re operating from guidance from CDC.”
Direction from federal health officials has, so far, been to focus almost exclusively on concerns around what amounts to cleanliness.



Megan Reynolds from El Cajon shopped at The Black in Ocean Beach on Saturday during the Memorial Day holiday weekend.
(Nelvin C. Cepeda / The San Diego Union-Tribune)
The term of art is “droplet transmission,” which refers to virus-laden moisture often expelled during a cough or sneeze that quickly falls to the floor. Droplets, technically speaking, are moisture bubbles larger than 5 micrometers, while the more buoyant aerosols are anything smaller.
Local health officials have pushed for aggressive hand washing and disinfecting of surfaces as a result of this thinking.
“We must continue to be vigilant with practicing hand hygiene, sanitation, face coverings, as well as social distancing, and screenings where appropriate,” Wooten said at the press event. “Practicing these strategies is going to be very important in maintaining and continuing to reopen our businesses.”
Prather and others in the aerosol science community don’t entirely disagree with that approach, but they’re concerned that such measures aren’t enough.
Researchers now widely believe that infected people can pass along the virus before they start showing any symptoms such as coughing or sneezing. As a result, aerosol scientists have questioned how droplets could be the dominant vehicle for transmission given the significant number of infections ascribed to asymptomatic individuals.
“People should be wary of crowded, indoor spaces and those with poor ventilation,” said Dr. Linsey Marr, an aerosol scientist at Virginia Tech and one of the country’s top experts on the airborne transmission of viruses.



Kate Marckese-Jass at One Door North in North Park takes a drink order from a group of friends celebrating their first dinner outing together since the coronavirus pandemic.
(Nelvin C. Cepeda / The San Diego Union-Tribune)
Marr and colleagues, such as Joseph Allen, director of the Healthy Buildings program at Harvard T.H. Chan School of Public Health, have warned for weeks about the risks of congregating indoors.
They’ve argued that spreading events, such as that of the Diamond Princess cruise ship in Japan, are not easily explained by close-contact, droplet transmission. They’ve said the spread of the virus in many instances outpaces what’s typical for non-airborne diseases.
They’ve also pointed to situations such as in March when one person was determined to have infected 52 of 60 members of a Washington state choir practice.
Local epidemiologists tracking the event said that droplet as well as aerosol transmission likely played a role in the contagion’s spread. Concerned researchers were quick to point out that singing emits as many aerosols as coughing.
What’s perhaps surprising is that those most worried about the airborne spread of the coronavirus have said addressing the issue is fairly straight forward.
“You might say that indoors is bad because it gets concentrated, but I would say in some ways indoors is good,” said Prather of UCSD. “The nice thing about indoors is you can change your airflow.”
Aerosol scientists are now teaming up with environmental engineers to outline best practices for ensuring that buildings are safe to return to. Those efforts include everything from limiting recirculated air to using portable air-filtering machines to zapping rooms with ultraviolet light.
Richard Corsi, dean of engineering and computer science at Portland State University and indoor-air-quality expert, said he’s currently focused on helping schools and universities retool their heating and air conditioning systems to prevent the potential spread of the virus.
“Recirculation basically means the dissemination of viruses if there are infectious viruses in aerosols in a building,” he said, “So one strategy is to terminate recirculation and bring in as much outdoor air as possible.”
That should be good news for San Diego officials and business people eager to get the economy back to normal without a new surge of virus infections.
“Every restaurant should open their windows if they have them,” said Charles Haas, professor of environmental engineering at Drexel University. “In San Diego, you’ve got the perfect climate for it.”



Diners eat on the rooftop at The Holding in Ocean Beach, which opened just in time for the Memorial Day holiday.
(Nelvin C. Cepeda / The San Diego Union-Tribune)

