According to British neurologists, COVID-19 can cause serious damage to the brain and central nervous system. Such damage can lead to psychosis, paralysis and strokes, which are often detected in their late stages.
There are numerous signs that the novel coronavirus SARS-CoV-2 not only attacks the lungs and respiratory tract, but also other organs on a massive scale.It can severely affect the heart, vessels, nerves, kidneys, and skin.
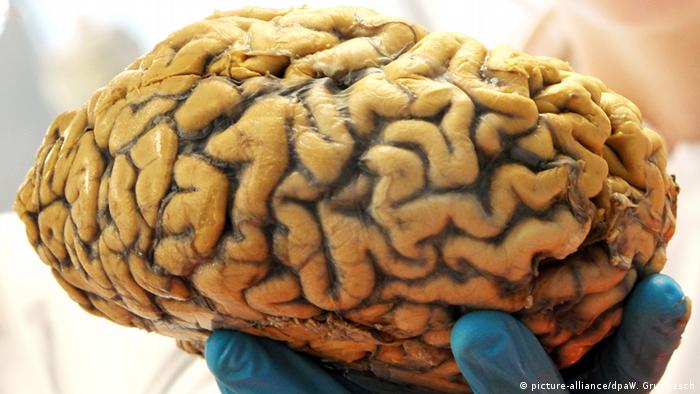
British neurologists have now published shocking details in the journal “Brain,” which suggests SARS-CoV-2 can cause severe brain damage — even in patients with mild symptoms or those in recovery. Often this damage is detected very late or not at all.
Neurologists at the University College London (UCL) diagnosed acute demyelinating encephalomyelitis (ADEM) in more than 40 British COVID-19 patients. This inflammatory disease causes a degenerative destruction of the central nervous system, affecting the myelin sheaths of the nerves in the brain and spinal cord.
Different degrees of damage
Of the patients examined, 12 suffered from inflammation of the central nervous system, 10 from a transient encephalopathy (brain disease) with delirium or psychosis, eight from strokes, and a further eight from problems of the peripheral nerves, mostly with the diagnosis of Guillain-Barré syndrome. This is an immune reaction that attacks the nerves and causes paralysis and is fatal in 5% of cases. A 59-year-old woman died of the complication.



Scientists have never before seen another virus attack the brain in the same way COVID-19 does, points out Dr. Michael Zandi. He is a lead author of the study, as well as a consultant at UCL Hospitals. What is unusual is the severe brain damage even in patients with mild symptoms.
Damage often goes unrecognized
The cases now published confirm fears that COVID-19 is causing long-term health problems in some patients. Many patients remain breathless and tired long after their recovery. Other recovering patients suffer from numbness, weakness, and memory problems.
Biologically, ADEM has some similarities to multiple sclerosis, but it is more severe and usually occurs only once. Some patients will be left with a long-term disability, while others will recover well, explains Michael Zandi.
The entire spectrum of brain diseases and long lasting side effects caused by SARS-CoV-2 may not yet have been recorded, said Zandi, because many patients in hospitals are too sick to be examined with brain scanners or other methods.



Neurological damage or late effects are partly not detected or are detected too late due to overload
Neurological damage or late effects are partly not detected or are detected too late due to overload
“We would like to draw the attention of physicians around the world to these complications of the coronavirus,” said Zandi. Physicians and medical staff should always consult a neurologist for patients with cognitive symptoms, memory problems, fatigue, numbness, or weakness.
Shocking case studies
Also published were touching individual stories, for example of a 47-year-old woman who suddenly felt headaches and numbness in her right hand after a week of coughing and fever. In the hospital she became fatigued and unresponsive. During an emergency operation, part of her skull had to be removed to relieve the pressure on her swollen brain.
Another 55-year-old patient without any previous mental illness began to behave strangely the day after being discharged from the hospital. For example, she put on and took off her coat several times in a row. She also began to hallucinate — seeing monkeys and lions in her house. Back at the hospital she was given antipsychotic medication.



The Spanish flu was an influenza pandemic that killed between 20 and 50 million people, according to the WHO
The Spanish flu was an influenza pandemic that killed between 20 and 50 million people, according to the WHO
Thousands of cases of brain damage, even with Spanish flu
British neurologists fear that COVID-19 could leave subtle brain damage in some patients, which will only become apparent in the coming years. According to the study, there were similar long lasting side effects discovered in those who recovered from the devastating Spanish flu in 1918, in which up to one million people probably suffered brain damage.
“Of course, we hope that this won’t happen, but when you have such a large pandemic affecting such a large part of the population, we have to be vigilant,” said Dr. Michael Zandi of the UCL Queen Square Institute of Neurology.
-


Seven facts about brain injuries
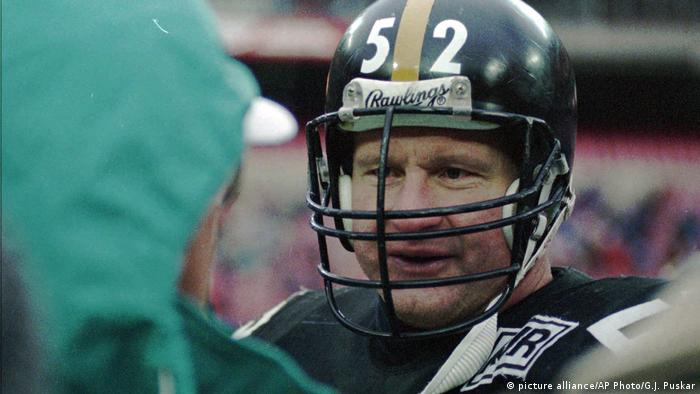
The NFL’s first CTE diagnosis
“Iron Mike” Webster won four Super Bowls as a center for the Pittsburgh Steelers in the 1970s. However, after his career ended, the many hits to the head that he had received as a football player took their toll on his health. He died in 2002 at the age of just 50. After his death, Webster was diagnosed as having had chronic traumatic encephalopathy (CTE), a neurodegenerative disease.
-



Seven facts about brain injuries
A Hollywood film
Bennet Omalu, a forensic neuropathologist (pictured above, second from left) was the first to diagnose CTE in Webster and other former NFL players. He continued his research despite widespread and strong resistance to his findings. In 2015 director Peter Landesmann (above, right) directed the film “Concussion,” in which actor Will Smith (left) played Omalu.
-


Seven facts about brain injuries
Gradual changes to the brain
Symptoms such as loss of speech, depression and dementia, which can be an indication of CTE, were first observed in boxers decades ago. Repeated blows to the head release the tau protein which accumulates in the brain. Those affected can experience changes to their personality, problems with aggression and even become susceptible to thoughts of suicide.
-



Seven facts about brain injuries
Suicide and a final wish
Between 2008 and 2015 Terry Long, Tom McHale, Jovan Belcher, Adrian Robinson and Junior Seau were among the former NFL players who committed suicide. In 2011, Dave Duerson, a former safety, shot himself through the heart instead of in the head. In his suicide note he asked that his brain be examined to see if he had CTE. Doctors found clear signs that he had had the disease.
-



Seven facts about brain injuries
The biggest stage
Head injuries occur in soccer as well. In the final of the 2014 World Cup in Rio de Janeiro, German midfielder Christoph Kramer was knocked out. He soldiered on for 14 minutes after the injury, which was a big risk, because a second hit shortly afterwards increases the danger of long-term damage. Even now, there is no universally agreed procedure for diagnosing brain injuries on the sidelines.
-



Seven facts about brain injuries
Risk varies by position
Brain injuries in soccer tend to occur when two players clash heads when going for ball or as the result of an elbow to the head. A recent study by the Federal Institute of Sports Sciences has found that the risk of head injury in soccer varies according to a player’s position. Defenders are most at risk, followed by midfielders and strikers. The risk is by far the lowest for goalkeepers.
-



Seven facts about brain injuries
Which is the worst sport for concussions?
A study conducted by the Federal Institute for Sports Sciences, showed that rugby players are at the highest risk among athletes of suffering concussion. They are followed by American football players, ice hockey players and basketball players. Brain injuries are not as common in soccer, but in Germany, where it is the biggest sport, in absolute terms, it is where the most concussions occur.

