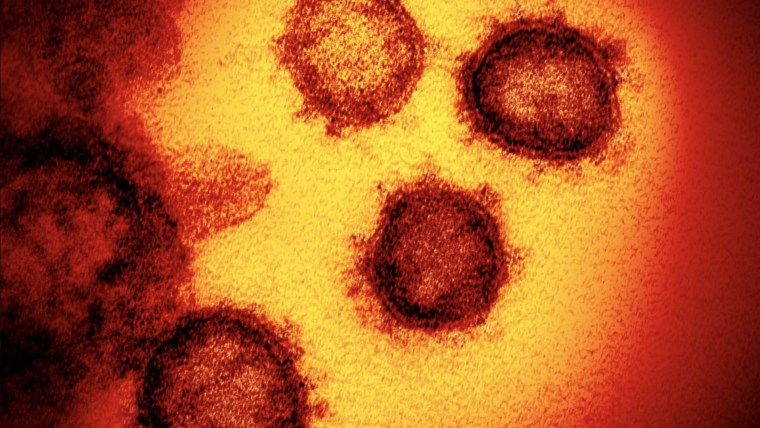
The results of a highly anticipated study on an experimental coronavirus treatment for the sickest patients are expected any day.
Physicians leading the clinical trial for the drug, called remdesivir, say the fast-moving pandemic has compelled them to work with haste, all without compromising the scientific rigor necessary to prove whether the drug really works.
Full coverage of the coronavirus outbreak
“We are in a race against time,” Dr. Andre Kalil, a principal investigator for the trial at the University of Nebraska Medical Center, told NBC News. “We’re doing everything we can 24/7 to make this happen.”
Previous research hinted at the promise of remdesivir, an antiviral drug that’s thought to work by blocking the virus from replicating itself in the body. But those studies were either based on animal data or had major caveats, such as lacking a control group.
A study published earlier this month in the New England Journal of Medicine found the drug improved breathing in some patients, but the study was small, with just 53 patients. And its authors did not compare their patients’ outcomes with a control group of patients to know for sure whether the improvements were truly due to remdesivir, or whether they would have become better on their own, without treatment.
The ongoing clinical trial at the University of Nebraska Medical Center, in partnership with dozens of other sites globally, does have a control group.
The trial is sponsored by the National Institutes of Health. Gilead Sciences, which developed the drug, is also involved.
Let our news meet your inbox. The news and stories that matters, delivered weekday mornings.
“This is something that we have to do as perfectly as possible,” Kalil said. “You have to have reliable data. It’s the soul of the whole study.”
Researchers must also carefully scrutinize any side effects that may be associated with the drug. Mild to moderate liver function abnormalities have been noted previously.
Beyond remdesivir
If remdesivir proves to be safe and effective against the coronavirus, Kalil said the trial will pivot to studying other drugs. The investigators would use remdesivir as the control, and see how well other drugs compare.
One treatment on deck is called baricitinib, an anti-inflammatory medication used to treat rheumatoid arthritis.
“There is hope that this medication can bring down inflammation and help prevent the spread of the virus from one cell to another,” Kalil said.
Download the NBC News app for full coverage of the coronavirus outbreak
A drug that can reduce inflammation may be key. The immune system naturally sends inflammatory chemicals to the site of an injury or infection in an attempt to fight it. But sometimes the immune system overreacts and fires off far too many, damaging otherwise healthy tissue.
Researchers are attempting to find the sweet spot of such inflammation — prompting the immune system enough to fight off the virus, but not overdo it.
Clinical trials for other treatments for COVID-19, the illness that results from the novel coronavirus, have also begun.
Drugmaker Alexion Pharmaceuticals has begun studies of Soliris (eculizumab), which is an immunosuppressant. And Roche is studying its arthritis drug, called Actemra (tocilizumab).
Another drug that has received attention is hydroxychloroquine, used to treat malaria. Trials studying the drug are underway, but the drug has not shown significant benefit so far in early studies.
Indeed, newly released COVID-19 treatment guidelines from a panel of experts within the National Institutes of Health declined to recommend any treatment — including remdesivir and hydroxychloroquine — for routine use because the scientific data aren’t available yet.
“At present, no drug has been proven to be safe and effective for treating COVID-19. There are insufficient data to recommend either for or against the use of any antiviral or immunomodulatory therapy in patients with COVID-19 who have mild, moderate, severe, or critical illness,” the panel wrote online.
Proof that a treatment works for COVID-19 would be a “game changer,” Dr. Michael Saag, associate dean for global health at the University of Alabama at Birmingham, said. Saag is not involved with any of the treatment trials.
“Once we know that, then we could mass produce it and have it available for every single person who starts showing symptoms, and then get it to them as soon as possible,” he said.
Follow NBC HEALTH on Twitter & Facebook.



Erika Edwards is a health and medical news writer and reporter for NBC News and “TODAY.”

